

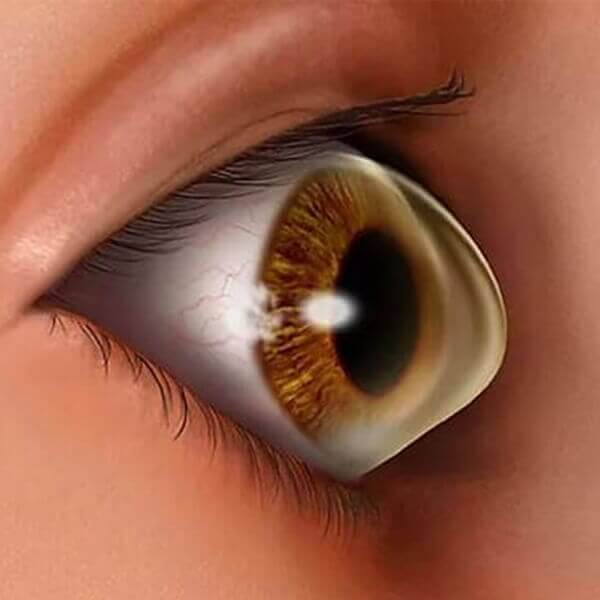
Keratoconus is a bilateral ocular disorder in which the cornea assumes a conical shape due to thinning of the stromal collage tissue.
It classically has its onset at puberty and is progreassive until the third or fourth decade of life when the disease usually arrests.
Treatment for Keratoconus depends on the severity of your condition and how quickly this condition can progress.
The two approaches to treating this condition is:
a. Slowing the progression
b. Improving your vision
If you use glasses or contact lenses to improve your sight, consider LASIK vision correction for the benefits.
One must have regular checkups from time to time to determine whether the fittings remain satisfactory. An ill fitting lens can damage your cornea.
In this procedure, the cornea is saturated with riboflavin eye drops and treated with ultraviolet light. This causes cross-linking of the cornea, which stiffens the cornea to prevent further shape changes. Corneal collagen cross-linking may help to reduce the risk of progressive vision loss by stabilizing the cornea early in the disease.
Newer advances for crosslinking include customized measurements of your cornea using your topography. We then use the laser to reduce corneal optical irregularities which causes the static and decreased visual function in the keratoconic eye. This target is achieved by incorporating your individual corneal topography map into the laser treatment. By utilizing your custom corneal corneal topography data, the laser reshapes your corneal surface to a more symmetric and rounder shape to improve the corneal optical architecture and visual performance. This is followed by corneal collagen crosslinking to give the necessary strength to the corneal bonds.
Acrylic rings are inserted in the corneal stromal to decrease the irregularity of the cornea. This can improve uncorrected vision without contact lenses.
This can also be followed by corneal collagen crosslinking to give the necessary strength to the corneal bonds.
In case of corneal corneal scarring, extreme thinning of your cornea, poor vision with the strongest prescription lenses or an inability to wear any time of contact lenses.
VissionTip : Transplant cases are generally very successful, but possible complications include graft rejections. Poor vision, infection and postoperative astigmatism.
